Have you ever wondered how mental health professionals keep track of their clients’ progress? Enter DAP notes – a powerful tool revolutionizing the way therapists document and analyze patient information. These notes are at the forefront of a documentation revolution, offering a structured yet flexible approach to capturing crucial patient data.
But what makes these notes so special, and why are they gaining traction in the mental health community? DAP notes provide a comprehensive solution for therapists seeking to enhance their clinical documentation practices and ultimately improve patient care.
In this comprehensive guide, we’ll dive deep into the world of DAP notes, exploring their benefits, structure, and practical applications. No matter your experience level in therapy, this guide will equip you with the insights and tools you need to elevate your patient records.
Read more: Medical Spa Software
What Is a DAP Note?
DAP notes, standing for Data, Assessment, and Plan, are a method used by mental health professionals to document client sessions in a structured and consistent way.
DAP notes provide a concise, organized way to document client interactions, progress, and treatment plans. They offer a snapshot of each session, facilitating better continuity of care and clearer communication between professionals.
While DAP notes share similarities with other documentation methods like SOAP and BIRP, they each have distinct characteristics:
Each method has its strengths and is suited to different contexts within mental health and healthcare settings. The choice of documentation method often depends on the specific needs of the practice, legal requirements, and the preferences of the mental health professional.
What Are the Benefits of DAP Notes?
DAP notes offer numerous advantages for mental health professionals:
- Improved Organization and Clarity:
The structured format helps clinicians keep information clear, concise, and well-organized, reducing the risk of omitting important details.
- Enhanced Communication:
DAP notes facilitate better information sharing among healthcare providers, ensuring continuity of care.
- Time Efficiency:
The streamlined format allows for quicker documentation compared to more complex systems, saving valuable clinical time.
- Legal Protection:
Well-written DAP notes serve as valuable documentation in legal situations, providing a clear record of the therapeutic process and clinical decision-making.
- Treatment Tracking:
The format makes it easy to monitor client progress over time, supporting evidence-based practice and treatment planning.
- Holistic Approach:
The integrated nature of DAP notes encourages a comprehensive view of the client’s situation, considering multiple aspects of their presentation and care.
- Flexibility and Adaptability:
DAP notes can be tailored to various mental health settings and therapeutic approaches, from brief interventions to long-term psychotherapy.
Read more: Progress Notes Examples
How to Write DAP Notes?
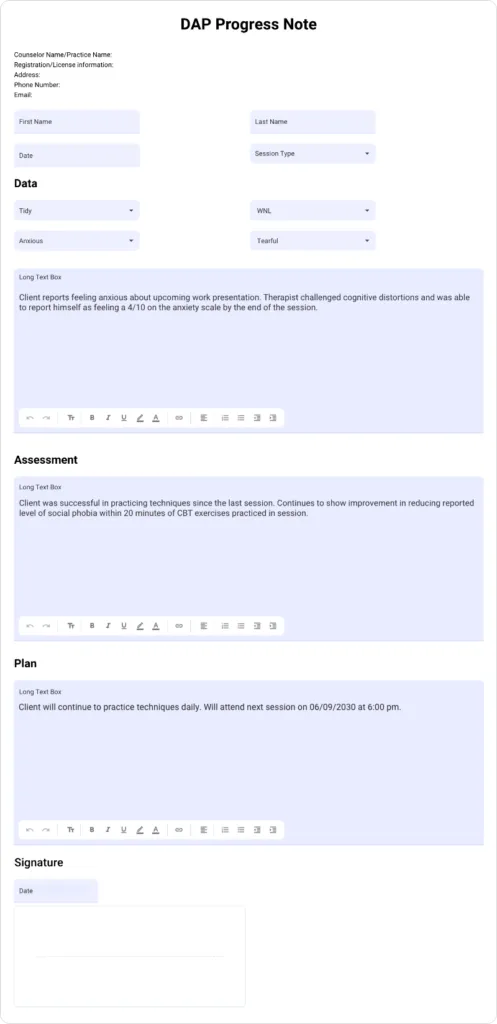
Writing effective DAP notes involves mastering each of the three components:
1. Data
The Data section includes both objective and subjective information gathered during the session:
- Record observable facts (objective data)
- Mention the mental status of the client as well as client’s appearance/hygiene
- Document the client’s statements and self-reports (subjective data)
- Use direct quotes when appropriate
- Avoid personal interpretations or judgments
- Include relevant measurable data (e.g., mood scores, physiological responses)
- Mention client’s presenting problem/reason for the session
- Note any significant changes in presentation or circumstances
- Record the time, date, and setting of the session
- Document the client’s level of participation or engagement
Example: “Session on 8/23/2024 at 2:00 PM in office. Client arrived 10 minutes late, appeared disheveled. Reported feeling ‘overwhelmed’ with work stress. Stated, ‘I haven’t slept well in days.’ PHQ-9 score: 14 (moderate depression). Client engaged actively throughout the 50-minute session.”
2. Assessment
In the Assessment section, analyze the data and provide your professional interpretation:
- Identify patterns or themes in the client’s behavior or statements
- Note any changes or progress since the last session
- Include your clinical impressions and hypotheses
- Mention how the client is progressing
- Relate observations to treatment goals and diagnostic criteria
- Consider differential diagnoses when appropriate
- Record the client’s diagnosis or any changes to their diagnosis
- Assess risk factors and protective factors
Example: “Client’s reported sleep difficulties, work stress, and elevated PHQ-9 score suggest worsening depressive symptoms. Progress towards the stress management goal appears to have stalled. No current suicidal ideation reported, but continued monitoring warranted. Client has made minimal progress on goal of establishing a regular sleep routine.”
3. Plan
The Plan section outlines the next steps in treatment:
- Specify interventions or techniques to be used in future sessions
- Set homework or assignments for the client
- Note any referrals or additional resources provided
- Indicate the focus for the next session
- Mention when the next session is, including the date and time
- Adjust treatment goals if necessary
- Consider medication referrals or consultations with other professionals
- Plan for crisis management if needed
- Outline SMART goals (Specific, Measurable, Achievable, Relevant, Time-bound) for future sessions
Example: “Introduce progressive muscle relaxation technique next session. Assign daily mood tracking and sleep hygiene practices as homework. Provide referral to sleep specialist if sleep issues persist. Discuss potential medication evaluation with psychiatrist. Next session: focus on developing a crisis safety plan. SMART Goal: Client will practice progressive muscle relaxation for 10 minutes daily and log sleep patterns for the next week. Next session scheduled for 8/30/2024 at 2:00 PM.”
Read more: Psychotherapy Notes vs Progress Notes
DAP Notes Examples
To better understand how DAP notes work in practice, let’s look at two examples:
Example 1: Depression
Data: Client arrived on time, dressed neatly. Reported feeling “slightly better” this week. Stated, “I managed to go for a walk every day, but I still struggle to enjoy things.” Sleep improved from 4 to 6 hours per night.
Assessment: Client shows minor improvements in mood and sleep patterns. Engagement in daily walks indicates progress in behavioral activation. Anhedonia persists, suggesting ongoing depressive symptoms.
Plan: Continue behavioral activation. Introduce pleasure prediction exercise for next week. Explore potential medication adjustment with psychiatrist.
Example 2: Anxiety
Data: Client appeared visibly tense, fidgeting throughout session. Reported increased panic attacks (3 this week vs. 1 last week). Stated, “I’m afraid to leave my house.” Breathing exercises helped “a little” during attacks.
Assessment: Client’s anxiety symptoms have intensified, with agoraphobic tendencies emerging. Breathing exercises show limited efficacy. Avoidance behaviors are reinforcing anxiety cycle.
Plan: Introduce cognitive restructuring techniques. Develop gradual exposure hierarchy. Increase session frequency to twice weekly for the next month.
DAP Notes in Various Mental Health Settings
DAP notes are versatile and adaptable to different mental health settings. The focus and content of these notes may vary depending on the specific environment and type of care provided. Here’s how DAP notes might be tailored for various settings:
a) Individual Therapy:
- Focus on personal goals, progress, and therapeutic alliance
- Track changes in symptoms, behaviors, and coping strategies
- Document interventions used and their effectiveness
b) Group Therapy:
- Note individual contributions, group dynamics, and cohesion
- Assess how each member responds to group interventions and peer interactions
- Document themes discussed and skills practiced during sessions
c) Family Therapy:
- Document family interactions, communication patterns, and alliances
- Track changes in family dynamics, individual roles, and problem-solving abilities
- Note family strengths and areas for improvement
d) School Counseling:
- Include academic performance, behavioral observations, and social interactions
- Note collaborations with teachers, parents, and other school staff
- Document interventions implemented and their impact on student well-being
e) Psychiatric Settings:
- Emphasize medication responses, side effects, and adherence
- Include risk assessments, safety planning, and crisis interventions
- Document changes in mental status and symptom severity
f) Substance Abuse Treatment:
- Track substance use patterns, triggers, and relapse prevention strategies
- Document participation in support groups and recovery activities
- Note progress in developing coping skills and lifestyle changes
g) Inpatient Psychiatric Units:
- Emphasize daily observations of behavior, mood, and functioning
- Document responses to milieu therapy and group activities
- Note discharge planning progress and aftercare arrangements
In all settings, DAP notes should maintain a focus on the client’s presenting problems, treatment goals, and progress while adhering to ethical and legal standards of documentation. The level of detail and frequency of notes may vary based on the intensity of care and regulatory requirements.
Tips for Writing DAP Notes
Writing DAP notes can be straightforward with the right approach. Here are some tips to ensure your notes are effective:
- Be concise yet comprehensive: Use clear, straightforward language while ensuring all essential information is captured.
- Maintain objectivity: In the Data section, report observable facts and client statements without personal interpretation.
- Use specific, descriptive language: Instead of vague terms like “seemed” or “appeared,” provide concrete observations with context.
- Focus on relevance: Include information directly related to the client’s presenting issues and treatment goals.
- Ensure consistency: Maintain a uniform format and level of detail across sessions for easy tracking of progress.
- Write promptly: Complete notes soon after the session to ensure accuracy and freshness of details.
- Employ professional terminology: Use appropriate clinical language and reference current diagnostic criteria (e.g., DSM-5).
- Review and revise: Proofread your notes for clarity, accuracy, and proper grammar.
- Structure your notes effectively:
- Begin with a brief summary of key observations.
- Include relevant direct quotes from the client to support your observations.
- Clearly outline any changes or adjustments to the treatment plan.
- Document risk and safety concerns: Always note any discussions or observations related to client safety, risk factors, or protective factors.
- Utilize technology: Use EHR systems for efficient documentation. Consider voice-to-text technology to dictate notes immediately during or after sessions.
- Create templates: Develop standardized templates within your EHR or note-taking system that follow the DAP format. This can streamline the documentation process and ensure consistency.
- Regular review: Periodically review your DAP notes to ensure they are effectively tracking client progress and informing treatment decisions. Use this review process to refine your note-taking skills and identify areas for improvement.
- Use SMART goals: When outlining plans, ensure goals are Specific, Measurable, Achievable, Relevant, and Time-bound.
Read more: How to Write Online Progress Notes 10X Faster
Challenges of Writing DAP Notes
While DAP notes offer many benefits, they also present some challenges:
Legal and Ethical Considerations in DAP Notes
Mental health professionals must navigate a complex landscape of legal and ethical requirements when documenting client sessions. Here are key considerations:
- Confidentiality: Ensure DAP notes contain only essential information and are stored securely. Avoid including identifying details about third parties.
- HIPAA Compliance: DAP notes must adhere to HIPAA regulations. This includes secure storage, controlled access, and proper disposal of records.
- Informed Consent: Clients should be aware of your note-taking practices. Include a discussion of documentation in your informed consent process.
- Record Retention: Familiarize yourself with state and professional guidelines on how long to keep client records.
- Subpoenas and Court Orders: Understand the legal process for responding to requests for client records, including when and how to release information.
- Cultural Sensitivity: Ensure your notes reflect cultural competence and avoid biased language or assumptions.
- Accuracy and Corrections: If errors are found in notes, follow proper procedures for amendments without altering the original record.
- Client Access: Be prepared for clients requesting to view their records, understanding both their rights and any applicable limitations.
Read more: Benefits of Electronic Therapy Notes
How to use DAP notes with your EHR
Integrating DAP notes into an Electronic Health Record (EHR) system can streamline the documentation process and improve accessibility. Many EHR systems allow customization of note templates, making it easy to incorporate the DAP format.
Yocale, an all-in-one solution for scheduling and business management, offers features that can complement your DAP note process, including digital forms and client management tools.
Conclusion
DAP notes are a valuable resource for mental health professionals, offering a structured yet flexible approach to clinical documentation. By mastering the art of writing effective DAP notes, clinicians can enhance their treatment planning, improve communication with colleagues, and ultimately provide better care for their clients.
As you implement DAP notes in your practice, remember that consistency and continual improvement are key. Regularly review and refine your note-writing process, and don’t hesitate to seek feedback from colleagues or supervisors.
The future of mental health documentation lies in efficient, clear, and client-centered approaches. By embracing DAP notes and integrating them with modern EHR systems, you’re not just improving your documentation – you’re taking a significant step towards enhancing the overall quality of mental health care.
FAQs
1. Can DAP notes be used in all mental health settings?
Yes, DAP notes are versatile and can be adapted to various mental health settings, including individual therapy, group therapy, family counseling, and psychiatric care.
2. How long should a typical DAP note be?
While there’s no strict rule, a typical DAP note should be concise yet comprehensive, usually ranging from 100-300 words depending on the complexity of the session.
3. Are DAP notes legally admissible?
Yes, well-written DAP notes can serve as legal documentation. It’s crucial to ensure they are accurate, objective, and comply with privacy laws and professional standards.
4. How often should DAP notes be written?
Ideally, DAP notes should be written after each client interaction or therapy session to ensure accuracy and timeliness of information.
5. Can DAP notes replace other forms of clinical documentation?
While DAP notes are comprehensive, they may not replace all forms of documentation. Some settings may require additional specific forms or assessments alongside DAP notes.
6. How do DAP notes differ from SOAP notes?
DAP notes differ from SOAP notes in structure and focus. While both formats are used for documenting client sessions, DAP notes consist of three sections: Data, Assessment, and Plan. SOAP notes, on the other hand, include Subjective, Objective, Assessment, and Plan. The key difference is that SOAP notes separate subjective client information and objective observations, while DAP notes combine these into the “Data” section, offering a more streamlined approach.
References
- Record Keeping Guidelines, American Psychological Association,
https://www.apa.org/practice/guidelines/record-keeping.pdf - How to write progress notes, Headway,
https://headway.co/resources/therapy-progress-notes - Counseling Treatment Plan, Thera Platform,
https://www.theraplatform.com/blog/406/counseling-treatment-plan - Guide to Creating Mental Health Treatment Plan, ICA Notes,
https://www.icanotes.com/2018/08/24/guide-to-creating-mental-health-treatment-plans/





